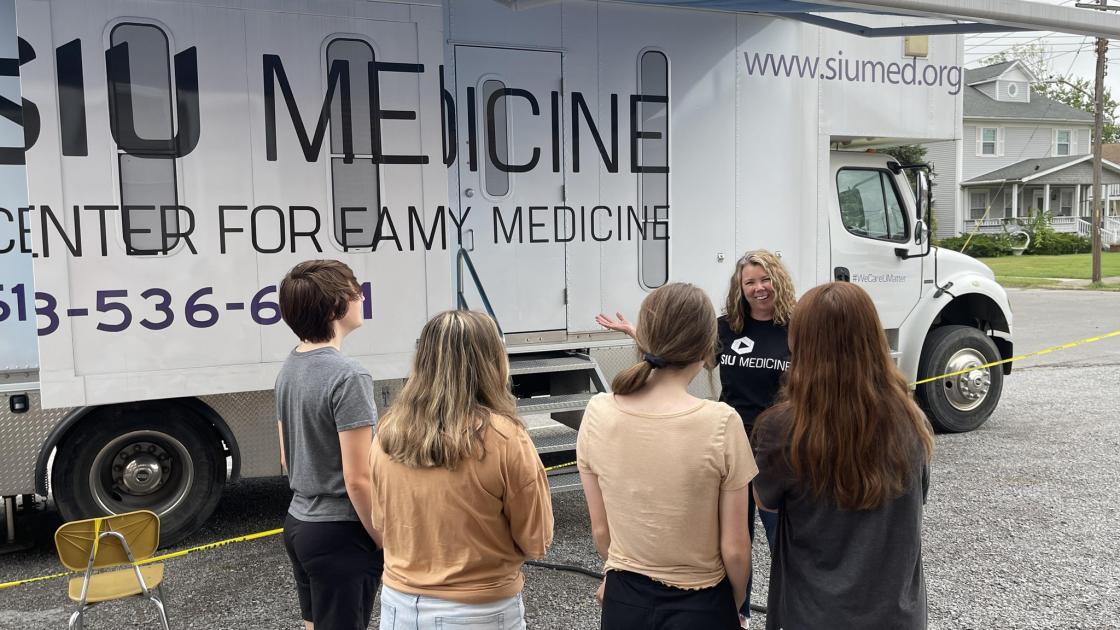
Care-A-Van delivers health care along rural routes
I met Jennifer Hammonds, LCSW, when I was in high school in West Frankfort, Ill., through her work on SIU School of Medicine’s Care-A-Van – a school health clinic on wheels that serves high schools in rural southern Illinois, including my alma mater. This is an edited version of our conversation about funding battles, the pandemic’s effects on issues mental and material and the overlooked importance of high-quality adolescent health care. - Olivia Weeks
What’s a Care-A-Van?
About 16 years ago our Carbondale area residency program director for Southern Illinois University School of Medicine’s Family Medicine, Dr. Penny Tippy, who was from West Frankfort – both of her sons went to West Frankfort high school – recognized that the adolescents in Franklin County did not have immediate access to mental health care or acute medical care. Illinois allows for some medical and counseling and substance abuse treatment without parent or guardian consent, but kids in the area just didn’t have access if they didn’t have parent or guardian support. So the idea of a Care-A-Van as a school-based health center was born out of that thought process: a mobile unit that would allow us to serve more schools in Franklin County.
Where did the funding come from to begin this program?
The van was about a million dollars to build, so it was quite a big investment for the medical school to put into the community. They began by applying for funding from the Illinois Department of Public Health, and the Illinois Children’s Health Care Foundation.

What type of services do the students have access to?
They began with Frankfort and Benton High School, and the Care-A-Van operated five days a week with a physician’s assistant, a registered nurse and a licensed clinical social worker. When I came on a year later as the new LCSW it was a very busy, active school-based health center. And at the time, we were the only mobile certified school-based health center in the state. Since that time, a lot of other mobile units developed, like dental vans, or dialysis vans. Although different mobile medical units have really taken off. We’re still unique in that we are certified by the Illinois Department of Public Health.
How have things changed over the years?
I think in the beginning we were a convenient care option that the school staff members used well. Having counseling full-time, which is still not very common in school-based health centers in general, was a big deal. We were seen as being beneficial for the students in reducing absenteeism, and it felt like everyone agreed that healthy kids equal healthy academics equal healthy communities. Gradually we began to create an even more robust understanding within the community of what the Care-A-Van really offers.
What do you do today?
Today we are well utilized at the schools that we’re at, and I honestly wish we could still operate five days a week because we’re not able to provide services to every school that has reached out. Students and staff have really relied on us being around post-pandemic. The mental health need is quite substantial for students who are coming back to a full-time school situation because maybe they have social anxiety after being at home, or maybe home might not have been safe or consistent throughout the pandemic. And so we’re seeing more trauma reactions, a lot of depression and anxiety. And that relates to what we’re seeing with more drug use and more housing instability and a lot more physical complaints. All these things seem to be tied together.
Why is the Care-A-Van necessary even though it may only serve a relatively small population?
IDPH indicated our funding grant is going to become “more competitive” based on data, so there is some concern among the rural school health centers. It is really hard to compare our utilization rates in small rural communities to those of the larger city schools. The northern part of the state is more urbanized, and they have some really amazing brick-and-mortar-style school health centers within the school building. Students can get a pass to go to the office and go to a wing of their high school that has a functioning clinic. Those health centers can see community members, not just students, and be really well-integrated into the school because they’re right there.
How does the population you serve differ from the larger cities?
We’re more spread out, less densely populated and though some adolescent health needs are universal, we can’t ignore that each area within the state has its own specific issues. Here, we are combating a lot of teen homelessness and methamphetamine use. If we see 20 kids a day, and the centers in Chicago and the Collar Counties see 200, we want to make sure that the value of both is recognized. Our students really benefit from having this kind of comprehensive health and medical care because they may not get it otherwise, especially when we’re talking about the number of students who are being currently identified as homeless, who don’t necessarily have a parent or guardian to consent for them to go to the doctor or to assist them in getting the services that they need. So being able to be on campus and working within state and federal law to provide these kids with services above and beyond what they could get in normal circumstances is really important to us.
In addition to the work you do with students, you’ve been involved in a lot of community engagement work over the years. What’s the goal for those broader efforts?
It’s not enough to just be in the van and be a provider. We need to be visible in community groups to show that we are invested in the community, because those things really correlate with the mission of the medical school and the Care-A-Van: to provide teen-friendly rural health care that’s specific to this particular population. I think it’s imperative for school health centers and people who work with adolescents to be aware of what is going on in our local communities because your mindset can get too narrow.

In Illinois, for example, heating costs have gone way up and our local energy assistance is out of funding until January. We’re seeing many families who may not be able to afford to heat their homes this winter, and then come January, funds will still be limited. That has come up repeatedly in our community groups. We’ve also had a bit of a housing crisis in our area. There seems to be less and less availability, so we’re finding more kids being shifted around to staying with family friends, or they’re staying with friends from school or in hotel rooms. We’ve also had a significant increase in the adult homeless population in the Franklin County area since the pandemic. It’s been daunting trying to return to normal.
Balancing individual cases against the larger needs in rural health care is a common challenge providers face. They are often structural in nature and much tougher to correct.
Yes, and it’s frustrating for those of us who work directly with families, because there’s only so much we can do. You really have to advocate to have systemic change and advocate politically to highlight the struggles that our families and kids are facing. I say this all the time: When we talk about childhood health care, we tend to think about younger, preschool children. Adolescents are often overlooked, just at a time when their health care and mental health care needs are really important. Adolescents carry a lot of stress; they’re under a lot of pressure. Many of them are taking on adult roles within their families, either helping financially or taking care of younger siblings. It can be a lot. So being there for them, one-on-one, and also looking at things on a wider macro level, is really essential for the health of our communities.
Reprinted with permission from The Daily Yonder’s Path Finders newsletter, November 28, 2022.
More stories from Aspects

Brenham named Associate Dean for Graduate Medical Education
Careyana Brenham, MD, has been selected as the new associate dean for graduate medical education (GME) at SIU School of Medicine. She succeeds Dr. Karen Broquet.

Cleaning, bonding, role modeling
For more than 10 years, SIU medical students have organized and volunteered for a “spring cleaning” day in the Enos Park and Pillsbury Mills neighborhoods. It’s fast becoming one of the more popular student-led traditions at SIU School of Medicine.

New program puts community health workers at ground level
Community health worker Kaye Barnes sports a purple SIU Medicine T-shirt to complement her green thumb as she works in Springfield’s community gardens.
